ServiceXG Basics
ServiceXG Basics
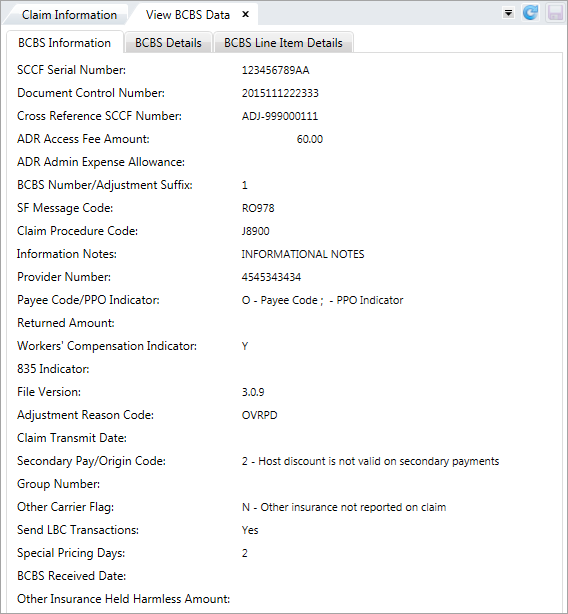
View BCBS data
The View BCBS Data option displays information about the currently selected BCBS claim, including line item details.
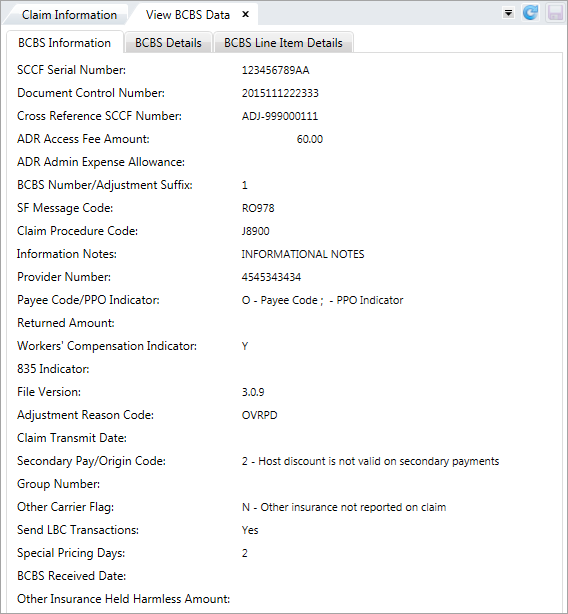
 BCBS Information Field Descriptions
BCBS Information Field Descriptions
SCCF Serial Number—A BCBS control number assigned to Labor BlueCard (LBC) claims only. Document Control Number—A BCBS control number assigned to BCBSIL (BlueCross BlueShield of Illinois) or HPA (Home Plan Aid Workstation) claims only. Cross Reference SCCF Number—A BCBSIL (BlueCross BlueShield of Illinois) control number for a billing change adjustment to a claim, if it was already paid or rejected. Applies to Labor BlueCard claims only. ADR Access Fee Amount—A fee charged per access to the BCBSIL (BlueCross BlueShield of Illinois) system. ADR Admin Expense Allowance—A fee per claim that BCBSIL (BlueCross BlueShield of Illinois) charges non-Illinois BCBS plans for administrative expenses. BCBS Number/Adjustment Suffix—Indicates the BCBS claim number (BCBS Number) and the number of adjustments on the claim (Adj Suffix).SF Message Code—A code that indicates whether something needs to be considered in adjusting the claim. Refer to your BlueCard Code Manual for SF message code definitions. Can indicate that a claim has a state prompt payment requirement. The following codes indicate a state prompt payment requirement might apply:P301- Prompt pay penalty applies to insured & ASO business.P302- Prompt pay penalty applies to insured business only. - P303- Prompt pay applies to international claims.
Claim Procedure Code—A code for the procedure performed. For institutional claims, this field contains either the HCFA Common Procedure Coding System (HCPCS) code or code needed as specified by each payer. If there isn't a procedure code, the field is left blank. For professional claims, the procedure is identified at the service level.Information Notes—Notes related to adjustments on Labor BlueCard claims.Provider Number—The unique number assigned to the provider for EMC identification purposes by the payer/receiver.Payee Code/PPO Indicator—Identifies the payee and payer of a claim (Payee Code) and the whether the provider in an Illinois (PPO Indicator).0—Payment to provider (BCBS to make payment)1—Payment to the member (Fund to make payment)2—Payment to third party (BCBS to make payment) 3—Payment to IL Dept. of Public Aid (BCBS to make payment) Y—Yes, this provider belongs to an Illinois PPO network. N—No, this provider doesn't belong to an Illinois PPO network. O—This provider is out of state.
Returned Amount—A credit/refund amount. WorkComp Indicator—Indicates whether the patient's condition was a result of a work-related accident (WorkComp) and whether the provider requires an electronic remittance (835 Indicator) for this claim. Y—Yes, the patient’s condition is a result of a work-related accident. N—No, the patient’s condition isn't a result of a work-related accident.U—Unknown.
835 Indicator—Indicates that the provider requires an 835 electronic remittance (835 Indicator) for this claim. Y—Yes, an 835 electronic remittance advice must be returned to the provider. N—No, an 835 electronic remittance advice isn't required.
File Version—The version of the file transmitted. Adjustment Reason Code—A BCBS code that represents an adjustment made to the original entry for a returned payment. Claim Transmit Date—The date the claim file was transmitted. SecondaryPay/OriginCode—Identifies whether BCBS plan’s discounts apply to secondary payments (Secondary Pay) and the origin of the claim. Secondary Pay applies to Labor BlueCard claims only. 1—Host discount is valid on secondary payments. 2—Host discount isn't valid on secondary payments. 3—Host discount. - Origin Code Values—Contact BCBS for a list of these codes.
Group Number—An ID number that represents the group or plan through which insurance is provided. Other Carrier Flag—Indicates whether the claim includes other carrier insurance information. Applies to Labor BlueCard (LBC) claims only. Y—Yes, the claim includes other carrier insurance information. N—No, the claim doesn't include other carrier insurance information. I—Other insurance is indicated; payment isn't known.
Send LBC Transactions—Indicates whether aLabor BlueCard claim is transmitted back to BCBS. Applies to Labor BlueCard (LBC) claims only. Y or —Yes, transmit the claim back to BCBS. N—No, don't transmit the claim back to BCBS.
Special Pricing Days—The number of days associated with the prompt payment requirement. See the SF Message Code field for additional information on prompt payment requirements. BCBS Received Date—The date the claim was originally received by the local BCBS plan. Use this as a start date in determining when the claim must be paid to meet the prompt payment requirement. See the SF Message Code field for additional information on prompt payment requirements.
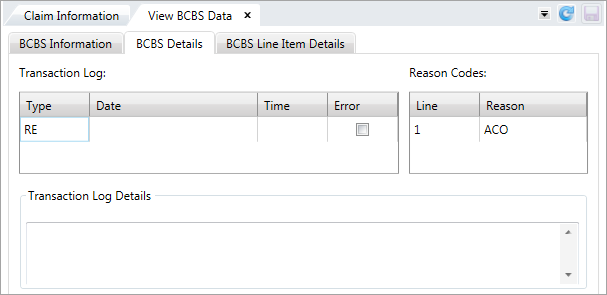
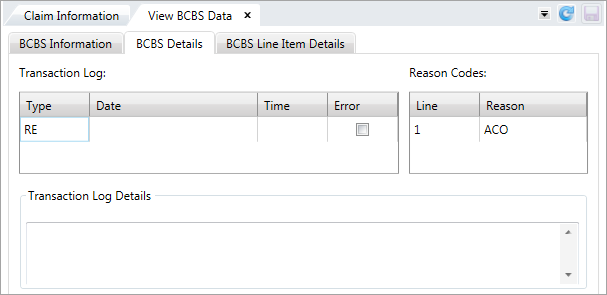
Use the transaction log to troubleshoot issues with any file transfer errors. The date, time, type of transfer and other details display here.
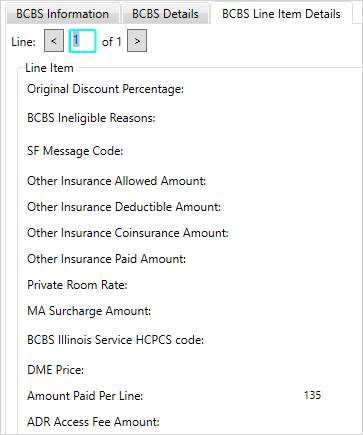
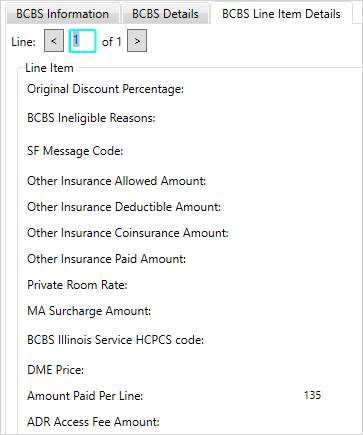
 BCBS Line Item Details field descriptions
BCBS Line Item Details field descriptions
Original Discount Percentage—The discount percentage applied to each line item. Applies to institutional claims only. BCBS Ineligible Reasons—A BCBS code that represents the reason a line item charge is denied. Contact BCBS for a list of ineligible codes. SF Message Code—A code that indicates whether something needs to be considered in adjusting the claim line items. Other Insurance Allowed Amount—The total payment amount covered under the other insurance carrier's contract. Applies to Labor BlueCard claims only.Other Insurance Deductible Amount—The other insurance carrier’s amount that the member must pay towards his or her medical expenses before benefits under the contract will be paid. Applies to Labor BlueCard (LBS) claims only. Other Insurance Coinsurance Amount—The other carrier’s coinsurance expense that the member is liable to pay under the contract. Other Insurance Paid Amount—The amount paid by other insurance carrier. Private Room Rate—The most common rate for a semi-private room. MA Surcharge Amount—A BCBSIL (BCBS of Illinois) surcharge amount for Massachusetts claims.BCBS Illinois HCPCS code—Health Care Financing Administration Common Procedural Coding System. A code for the procedure performed.Amount Paid Per Line—Amount that has been adjusted via Universal Adjustment process or using Reverse/Void Processes. ADR Access Fee Amount—A fee charged to access to the BCBSIL (BCBS of Illinois) system.
 SEE ALSO
SEE ALSO
![]() BCBS Information Field Descriptions
BCBS Information Field Descriptions